There are hundreds of eye diseases which can lead to problems with vision and if not identified or treated early enough, can even lead to blindness. Orthoptists are the experts in identifying, diagnosing and treating defects in eye movement and problems with how the eyes work together, with roughly 1,100 practising orthoptists in the UK. Orthoptists also work with patients with a range of neurological conditions such as Stoke and Parkinson’s disease, based on the brain’s relationship with our eyes.
The University of Liverpool is one of only three universities across the UK that offer an Orthoptics BSc (Hons) degree. Students are equipped with the necessary skills to diagnose and manage conditions which may be present within a range of patients from infants to the elderly.
These can include strabismus disorders (eye misalignments), amblyopia (sometimes called lazy eye), traumatic injuries, tumours, head injuries, diabetes, and strokes. Students focus on the fundamentals of the nervous system, neuroanatomy, and physiology, and where it relates to the practice of orthoptics.
THE CHALLENGE
As part of the course, students are required to go on clinical placements to gain hands-on experience. These placements are limited in terms of time frame and exposure to specific eye conditions. Therefore, there is a need to allow students to familiarise
themselves with the ‘tools of the trade’ and have some experience in diagnosing patients before their clinical placement; allowing them to better utilise their placement.
THE SOLUTION
The University department of Orthoptics had previously engaged with the Virtual Engineering Centre (VEC) and was aware of previous collaborations across the University. The Orthoptics team approached the VEC to see how immersive learning technologies could be applied for improving the realism of the simulations and how students could use this as an educational tool.
The VEC team developed a more realistic simulation where the user is immersed within a virtual studio or inspection room, using high-fidelity Virtual Reality (VR). These high levels of quality graphics can improve outcomes, whilst making the learning
experience more enjoyable for students.
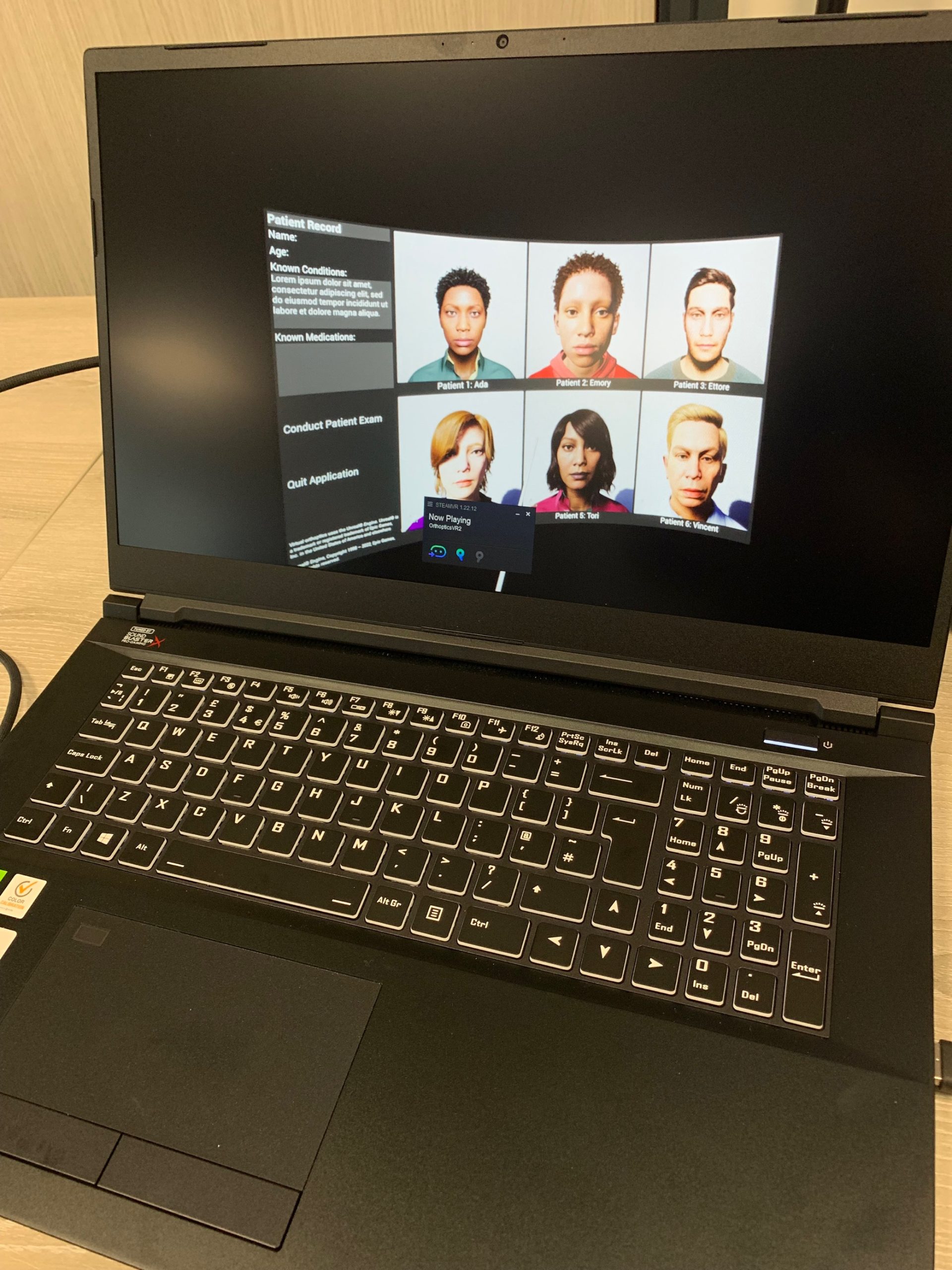
The VR simulation has also been created to include Metahumans who have an array of different eye conditions. Students can support and assess each patient whilst using a variety of popular and virtual orthoptics tools including a torch, prism sticks, snellans sticks and glasses which can support the virtual diagnosis of patients. This higher level of fidelity allows the simulation of realistic corneal reflections, which is a very important aspect in diagnosing specific eye conditions.
The VEC developed the simulation in stages, keeping regular updates and communication with the orthoptics teams, and gaining valuable feedback to ensure it was as realistic as possible for their working environment. This included the range of
different tools to be included and the different types of eye conditions, adding greater variety for a further improved experience.
THE IMPACT
The VEC created the bespoke simulation to meet the needs and requirements of the orthoptics teams. The realism of the simulation will now enable students to gain key observational and diagnostic clinical skills and outline treatment plans for even
more eye conditions which can be easily flagged and identified, enabling earlier treatment.
This engaging interactive teaching tool has already been implemented and used by over thirty students with the hope to extend even further in the near future.
Overall, the plan is to embed this valuable clinical resource within the curriculum to support students in clinical development, increasing their accessibility so every orthoptic student can use it at least once during their studies.
In addition to this simulation, the VEC team created a video to showcase how the simulation works, how it can be used and to highlight realism, which is a huge improvement to previous methods and the use of a simple 2D application.
The orthoptics team have since used this video as a communication and marketing tool which resulted in the team winning a Learning and Teaching Fellowship, an internal University award which can support further funding research and
teaching, available to a few selected individuals.
Initially I thought the simulation would be really hard to use and navigate, however it enabled us to see a real patient with a real condition and having the time to undertake and manage the tests which have really added value.
– Orthoptics student, University of Liverpool